News and Announcements
Volume 3 Issue 1 2022
Order by
Download Full Issue
Latest time
REVIEW
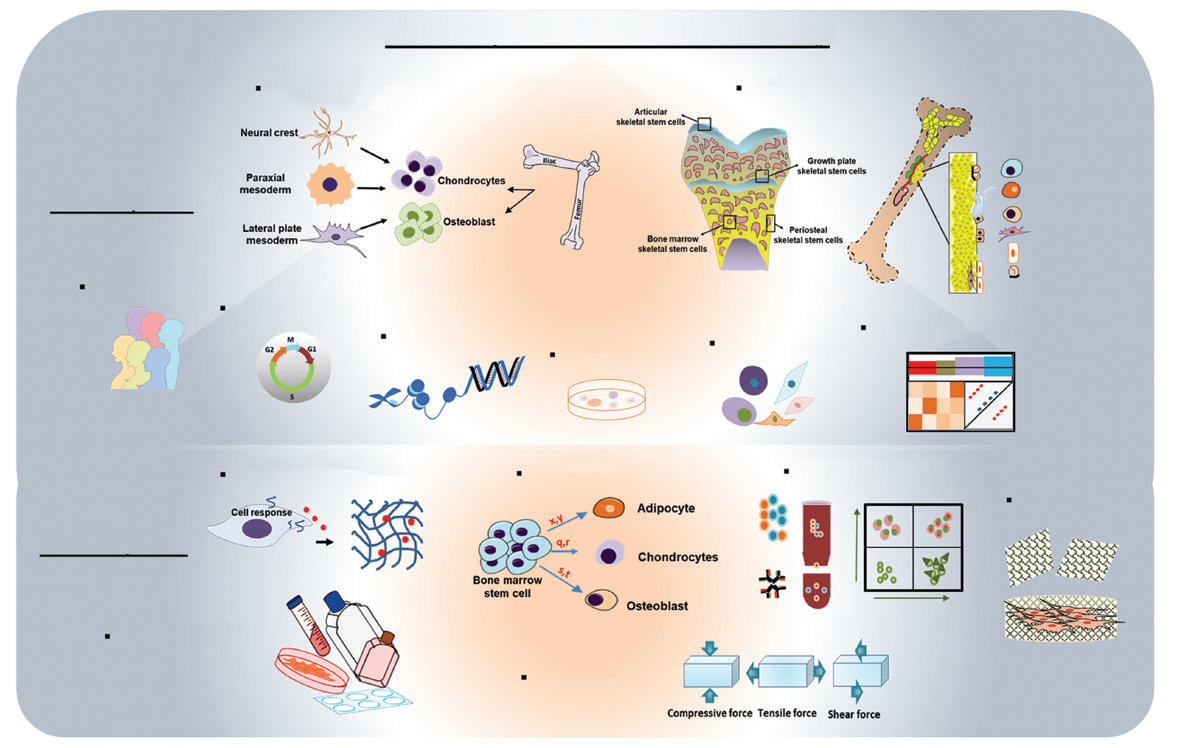
Recent updates on the biological basis of heterogeneity in bone marrow stromal cells/ skeletal stem cells
Deepika Arora,
Pamela Gehron Robey
6 Download 1155 Views
REVIEW
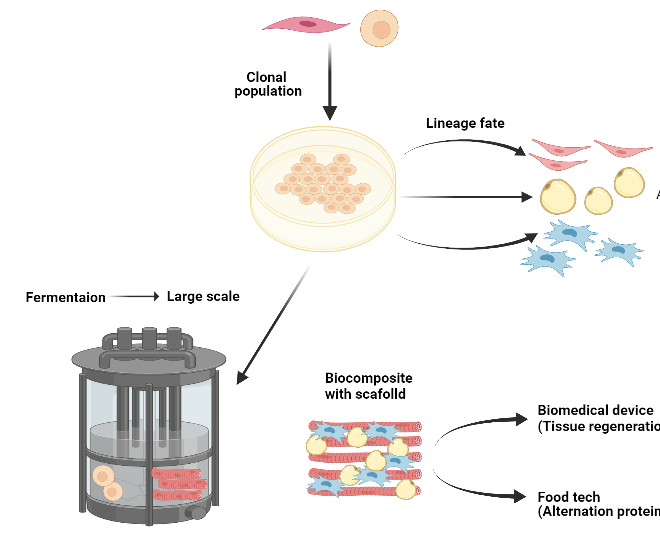
Mesenchymal stem cell differentiation and usage for biotechnology applications: tissue engineering and food manufacturing
Deepika Arora,
Pamela Gehron Robey
14 Download 1452 Views
REVIEW
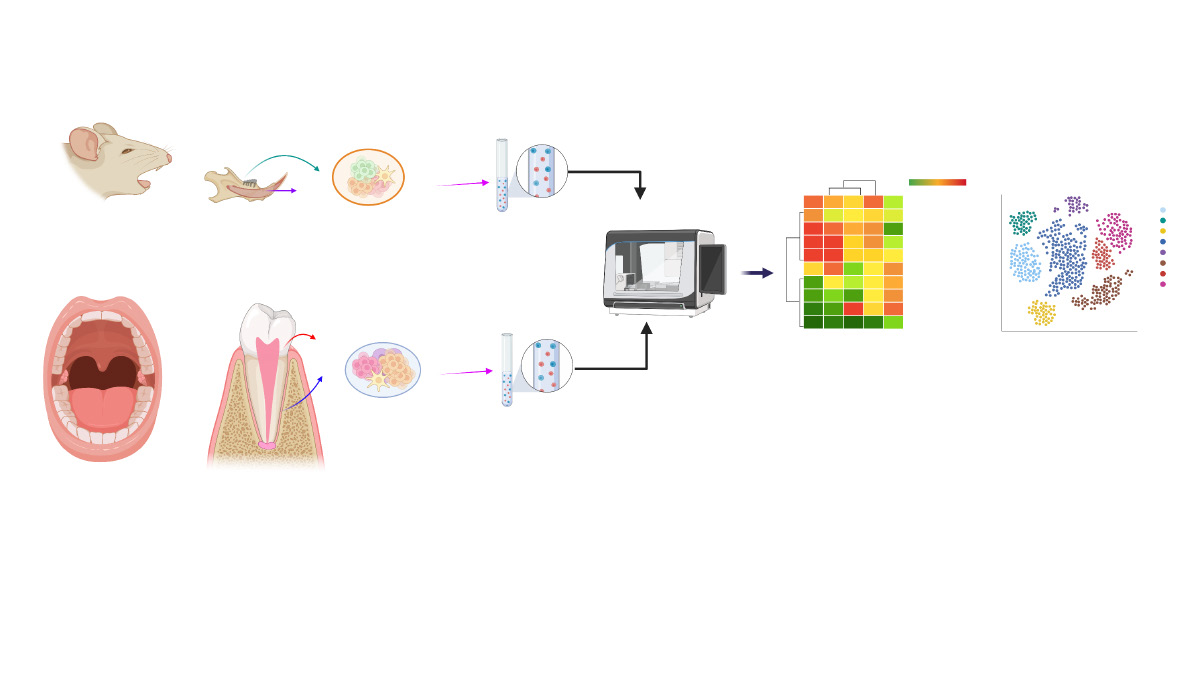
Oral stem cells, decoding and mapping the resident cells populations
Xuechen Zhang,
Ana Justo Caetano,
Paul T. Sharpe,
Ana Angelova Volponi
20 Download 1566 Views
REVIEW
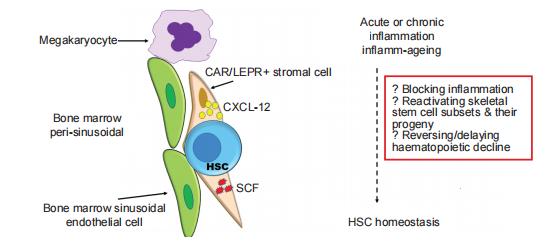
The long and winding road: homeostatic and disordered haematopoietic microenvironmental niches: a narrative review
Suzanne M. Watt
7 Download 1298 Views
REVIEW
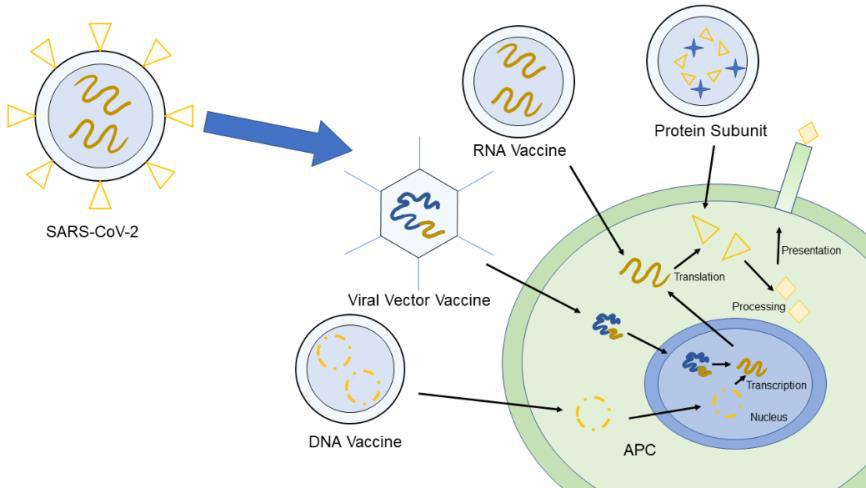
A biomaterials viewpoint for the 2020 SARS-CoV-2 vaccine development
Isak Jatoi,
Jingyu Fan
1696 Views
REVIEW
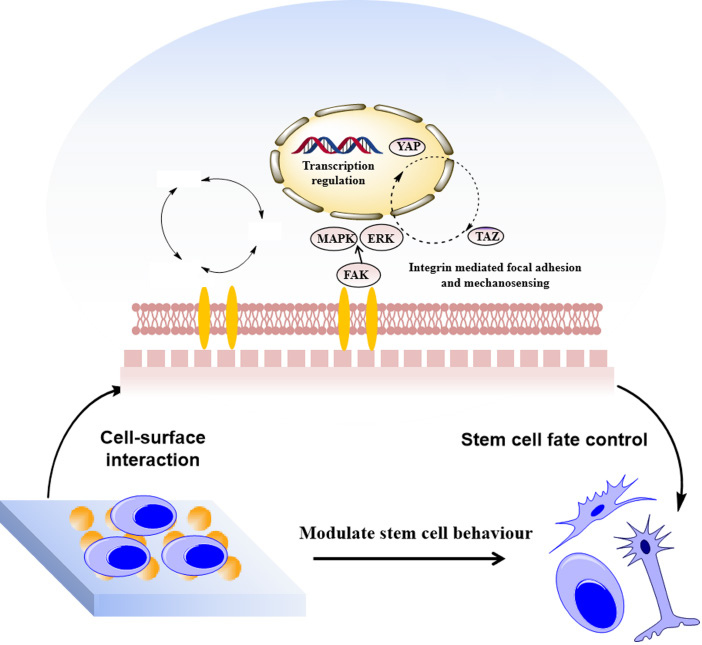
An update of nanotopographical surfaces in modulating stem cell fate: a narrative review
Shuqin Cao,
Quan Yuan
7 Download 1489 Views
REVIEW
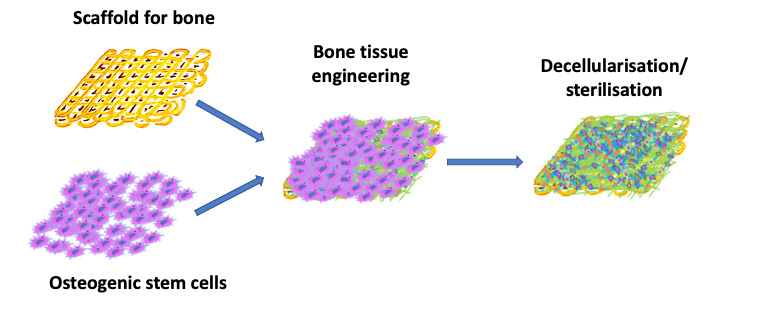
Manufacturing artificial bone allografts: a perspective
Emma Steijvers,
Armaan Ghei,
Zhidao Xia
42 Download 2904 Views
REVIEW
History, progress and future challenges of artificial blood vessels: a narrative review
Ke Hu,
Yuxuan Li,
Zunxiang Ke,
Hongjun Yang, ... Weici Wang
107 Download 2814 Views



